Decoding Chronic Pelvic Pain Syndrome in Men: Recognizing the Telltale Signs
Unraveling the Mysteries of Chronic Pelvic Pain Syndrome in Men, commonly known as non-bacterial prostatitis. Understanding the symptoms of CPPS is crucial in distinguishing it from other conditions such as bacterial infections or prostate cancer. Antibiotics are not always the solution for treating this chronic condition, highlighting the importance of accurate diagnosis and targeted medical interventions within urology. Explore the intricate web of symptoms, causes, and treatment options for individuals experiencing the debilitating effects of CPPS.
Understanding Chronic Pelvic Pain Syndrome in Men
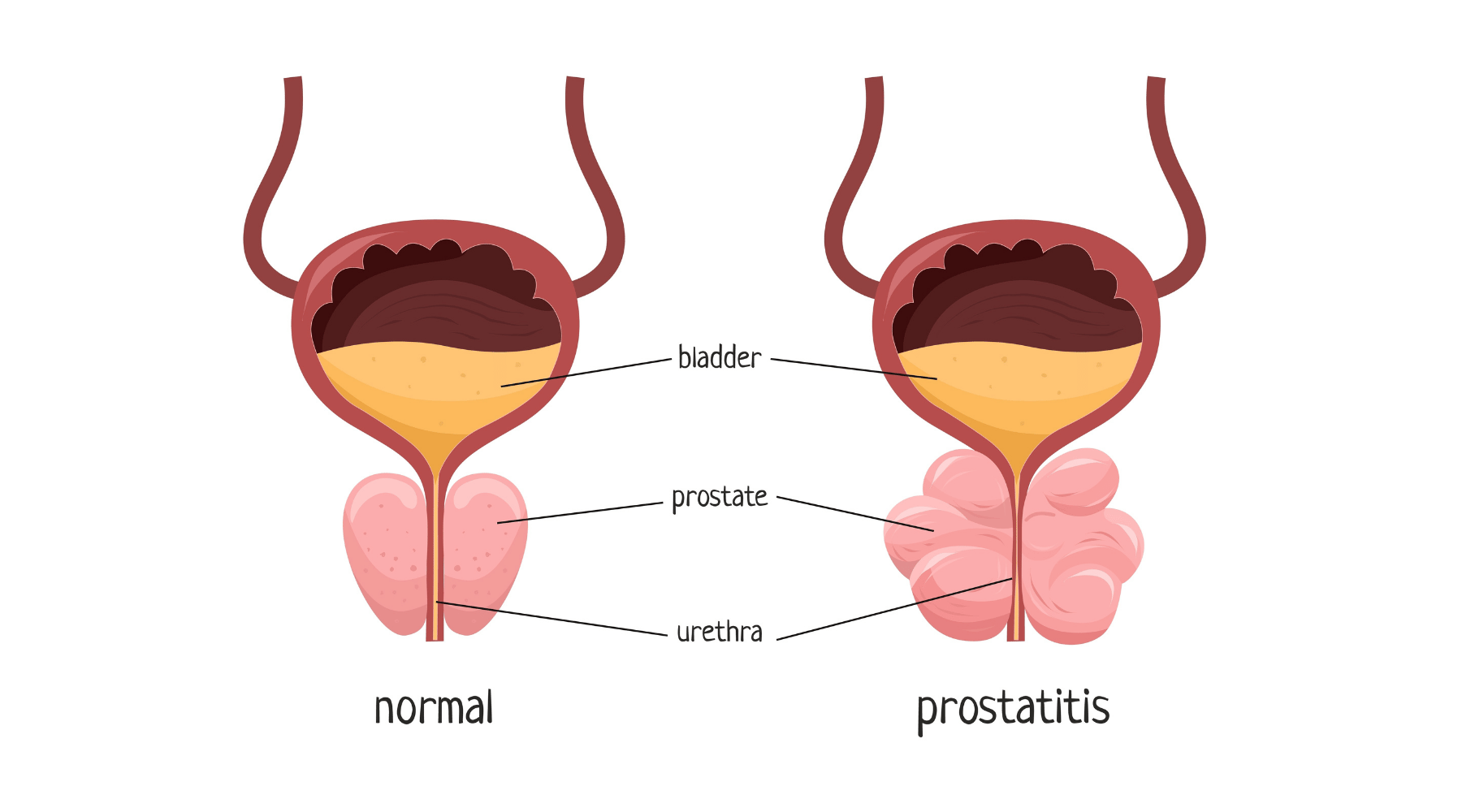
In the realm of chronic pelvic pain syndrome in men, the symptoms of non-bacterial prostatitis can often mimic those of a bacterial infection. This can lead to misdiagnosis and unnecessary antibiotic treatments. It's crucial for men experiencing pelvic pain to seek medical evaluation to determine the underlying cause of their discomfort. While non-bacterial prostatitis is not linked to cancer, its chronic nature can significantly impact a man's quality of life. Urology professionals play a key role in diagnosing this syndrome and guiding patients towards appropriate treatment options. Understanding the distinct characteristics of CPPS non-bacterial prostatitis is essential for effective management and symptom relief. By empowering men with knowledge about their condition, we can enhance their ability to recognize and address the symptoms of this challenging syndrome.
Identifying Symptoms of CPPS Non-Bacterial Prostatitis
Recognizing the symptoms of CPPS non-bacterial prostatitis is crucial for early detection and effective management. Unlike bacterial prostatitis, this chronic syndrome is not caused by infections and does not respond to antibiotics. Common symptoms include pelvic pain, urinary issues, and discomfort during ejaculation. It's essential to differentiate CPPS from other conditions like prostate cancer to receive appropriate medical care. Urology specialists use diagnostic tools such as urine tests and pelvic exams to confirm a nonbacterial prostatitis diagnosis. Treatment options focus on alleviating pain and improving quality of life through medications, physical therapy, and lifestyle adjustments. By understanding the telltale signs of CPPS non-bacterial prostatitis, men can proactively address their symptoms and seek tailored care for long-term relief.
Diagnostic Tools for CPPS Non-Bacterial Prostatitis
When it comes to diagnosing CPPS non-bacterial prostatitis, medical professionals rely on a variety of diagnostic tools to pinpoint the exact cause of pelvic pain. These tools may include urine tests to rule out infections, prostate exams to check for abnormalities, and urological evaluations to assess urinary function. It's crucial to differentiate between bacterial and nonbacterial causes, as treatment approaches vary significantly. While antibiotics are effective for bacterial prostatitis, they are not the appropriate solution for non-bacterial cases. By undergoing these diagnostic tests, individuals with CPPS can receive an accurate diagnosis and personalized treatment plan tailored to their specific symptoms. Early detection and proper diagnosis are key in effectively managing chronic pelvic pain syndrome in men and improving their overall quality of life.
Treatment Options for Managing Symptoms
Exploring treatment options for managing symptoms of CPPS non-bacterial prostatitis involves a multifaceted approach. While antibiotics are ineffective due to the absence of a bacterial infection, medical professionals may recommend therapies focusing on pain management and pelvic muscle relaxation. Urology specialists can provide guidance on urinary symptoms and offer strategies to alleviate discomfort. It's crucial to address the chronic nature of CPPS and tailor treatments to each individual's needs. Alternative therapies, such as physical therapy or acupuncture, may complement traditional medical interventions. The use of natural remedies, like Prostasolv quercetin combination supplements that help regulate inflammation and relieve pain are also recommended.
By consulting with healthcare providers knowledgeable about CPPS, men can navigate the array of available treatments and find a personalized plan to improve their quality of life. Empowerment lies in understanding the diverse treatment modalities and proactively engaging in self-care practices to combat the challenges posed by this syndrome.
Lifestyle Changes and Self-Care Strategies for CPPS Non-Bacterial Prostatitis
Implementing lifestyle changes and self-care strategies is crucial for managing symptoms of CPPS non-bacterial prostatitis. While antibiotics are ineffective against this nonbacterial condition, medical professionals recommend a holistic approach to alleviate pelvic pain and urinary issues. Regular exercise, stress management techniques, and a balanced diet can play a significant role in symptom relief. Additionally, maintaining a healthy weight and avoiding alcohol and caffeine can help reduce inflammation in the prostate region. Seeking guidance from a urology specialist is essential to tailor a treatment plan that addresses individual needs. By incorporating these lifestyle adjustments, men can empower themselves to take control of their health and enhance their overall well-being in the face of chronic pelvic pain syndrome.
Conclusion: Empowering Men to Recognize and Address CPPS Symptoms
Empowering men to recognize and address symptoms of CPPS non-bacterial prostatitis is crucial for effective management. While antibiotics may be ineffective due to the absence of bacterial infection, understanding the chronic nature of this syndrome is key. Symptoms such as pelvic pain, urinary issues, and discomfort can often be misinterpreted, leading to delayed treatment. Seeking medical advice for accurate diagnosis and tailored treatment options is essential. By addressing the root cause, which may not involve infection or cancer, men can take proactive steps towards alleviating pain and improving quality of life. Urology professionals play a vital role in guiding individuals towards appropriate care and lifestyle adjustments to manage CPPS effectively. It's time to empower men with knowledge and resources to tackle CPPS non-bacterial prostatitis head-on.
People also ask
What are the symptoms of non bacterial CPPS?
Non bacterial chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterized by symptoms such as pelvic pain, discomfort in the genital area, urinary frequency and urgency, pain during or after ejaculation, and pain in the lower back or abdomen. Other symptoms may include difficulty or pain with urination, erectile dysfunction, and discomfort while sitting for long periods. Additionally, individuals with non bacterial CPPS may experience fatigue, muscle aches, and emotional distress such as anxiety or depression. These symptoms can vary in intensity and may come and go over time. It is important for individuals experiencing these symptoms to seek medical evaluation and diagnosis to determine the underlying cause and appropriate treatment plan.
Can non bacterial prostatitis cause testicular pain?
Non-bacterial prostatitis can indeed cause testicular pain. In some cases, the inflammation and irritation in the prostate gland can radiate pain to the surrounding areas, including the testicles. This can result in discomfort, soreness, or even sharp pain in the testicular region. The proximity of the prostate gland to the testicles can lead to referred pain, where the sensation is felt in a different location than the actual source of the issue. It is important to consult a healthcare provider for proper diagnosis and treatment of non-bacterial prostatitis if testicular pain is present. Pain management strategies, lifestyle changes, and medication may be recommended to alleviate symptoms and improve overall quality of life. Regular communication with a healthcare professional can help effectively manage and address any discomfort or pain associated with non-bacterial prostatitis.
How long can nonbacterial prostatitis last?
Nonbacterial prostatitis can last for a variable period of time, ranging from weeks to months or even years. The duration of the condition can be influenced by factors such as the individual's overall health, the effectiveness of treatment, and lifestyle changes. In some cases, nonbacterial prostatitis may resolve on its own over time, while in others, it may require ongoing management to control symptoms and prevent flare-ups. It is important for individuals with nonbacterial prostatitis to work closely with their healthcare provider to develop a personalized treatment plan that addresses their specific needs and aims to improve their quality of life. Regular follow-up appointments and monitoring may be necessary to track progress and make any necessary adjustments to the treatment plan. Overall, the duration of nonbacterial prostatitis can vary from person to person, and a proactive approach to managing the condition is essential for long-term health and well-being.
Can non-bacterial prostatitis cause back pain?
Non-bacterial prostatitis can indeed cause back pain. The inflammation and swelling of the prostate gland in non-bacterial prostatitis can lead to referred pain in the lower back. The close proximity of the prostate gland to the nerves and muscles in the lower back can result in discomfort and pain in this area. Additionally, the inflammation in the prostate can cause pressure on surrounding structures, leading to radiating pain in the back. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan if you are experiencing back pain associated with non-bacterial prostatitis.